Acute pancreatitis
CHIEF COMPLAINTS-
C/o itchy skin lesion on left foot since 10 yrs which initially started as a papule
C/o pain in the abdomen since 3 days
C/o constipation since 3days
C/o vomitings since 2days
HISTORY OF PRESENT ILLNESS-
Pt was apparently asymptotic 2days ago then he developed pain in the abdomen-epigastric region. Pain is sudden in onset, gradually progressive. Pain increases more after eating food and on lying in supine position. Pain is relieved on sitting position and on bending forward.
H/o 3 episodes of vomiting yesterday after eating food. Content- food, non bilious, non projectile, not blood tinged. Constipation since 3days
No h/o fever , cough , cold, SOB, loose stools, giddiness
HISTORY OF PAST ILLNESS-
Last binge of alcohol consumption 2days ago
H/o similar complaints 2yrs ago diagnosed as acute pancreatitis.
No H/o diabetes mellitus, hypertension, thyroid disorders,TB,CAD,CVBA, Epilepsy
TREATMENT HISTORY-
Application of unknown topical medication on skin lesions .
PERSONAL HISTORY-
Appetite- normal. Non-vegetarian
Bowel- constipation
Micturition- normal
Addictions-
Alcohol- consumes 2 quarters alcohol/day
Smoking- nil
No h/o drug abuse
FAMILY HISTORY-
Father is an alcoholic
PHYSICAL EXAMINATION-
GENERAL EXAMINATION-
No signs of pallor, icterus, cyanosis, clubbing of fingers, lymphadenopathy, oedema, dehydration
VITALS-
Temperature- 97.8
Pulse rate- 76/min
Respiration rate- 18/ min
BP- 110/80 mm Hg
SPO2- 96%
GRBS- 124mg %
SYSTEMIC EXAMINATION-
CVS-
Thrills- No
Cardiac sounds- s1s2 heard
Cardiac murmurs- No
RESPIRATORY SYSTEM-
Dyspnoea- no
Wheeze- no
Position of trachea- central
Breath sounds- vesicular
ABDOMEN-
Shape of abdomen- scaphoid
Tenderness- no
Palpable mass - no
Hernial orifices - normal
Free fluid- no
Bruit- no
Liver- not palpable
Spleen- not palpable
Bowel sounds- present sluggish 2mins
CNS- pt is conscious coherent and afebrile on touch
Level of consciousness- conscious
Speech- normal
Glasgow scale- E4, U5, M6
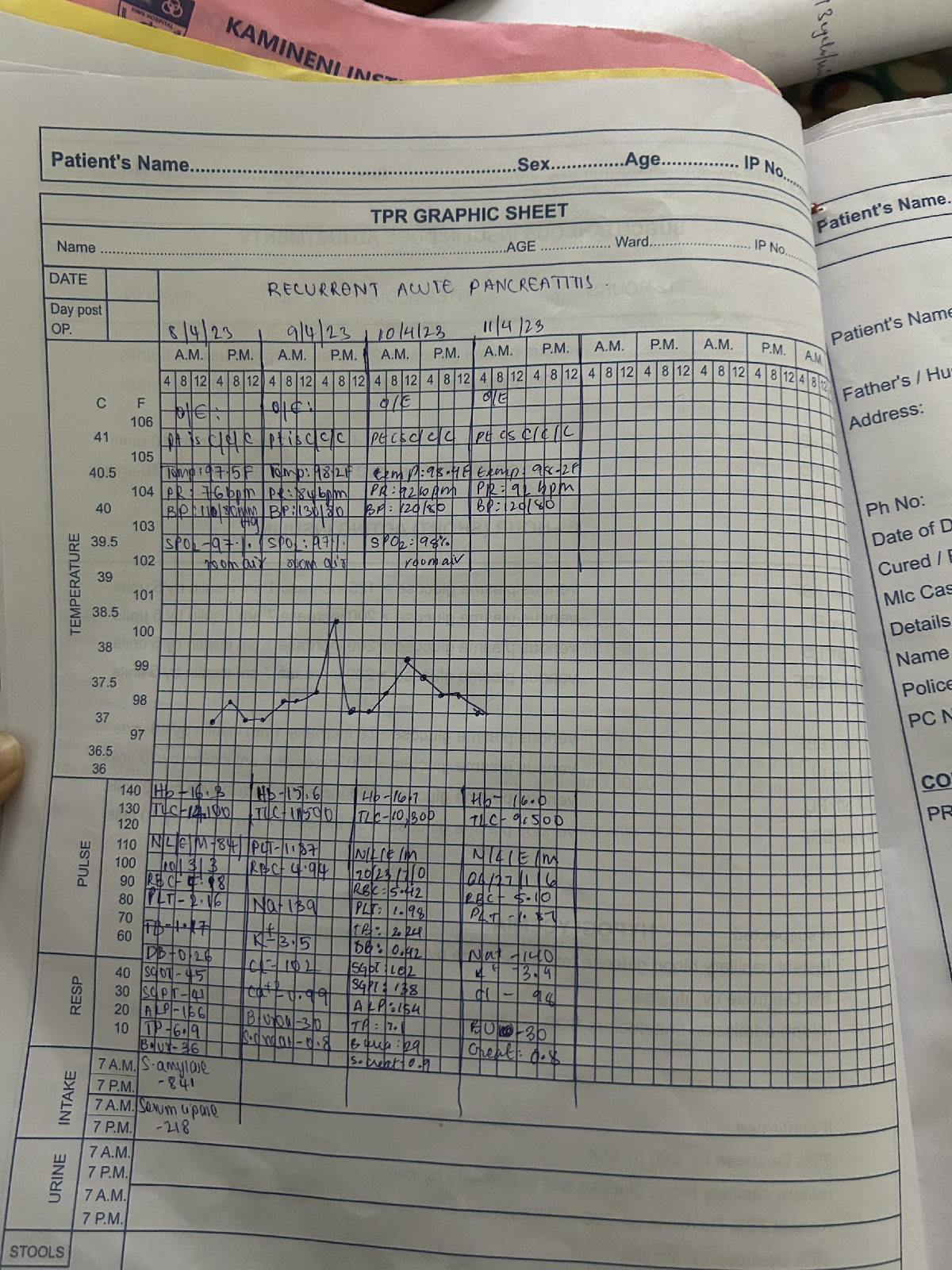
Fever chart
INVESTIGATIONS:
HAEMOGRAM
CUE
2D ECHO
UlTRASOUND
ECG

Acute pancreatitis
TREATMENT-
NBM till further order
IV fluids
Inj. TRAMADOL 1 amp in 100 ml NS in IV
Inj THIAMINE 1 amp in 200 ml NS IV BD





Comments
Post a Comment